Breast Cancer

We understand a breast cancer diagnosis is a challenging and emotional journey filled with uncertainty and countless questions. Our team of specialists will be by your side through it all. You can expect to receive our all questions answered, exceptional expertise and know how much I matter kind of care.
The second most common cancer for women in the United States, although men can develop it too, breast cancer begins to grow in the cells of one of both breasts. Signs of breast cancer don’t always start with a lump and can also show up as subtle changes in the breast tissue. However, it’s important to note that most breast lumps are benign (not cancerous), but some types of benign breast lumps can increase your risk of getting breast cancer.
Breast cancer survival rates have been steadily increasing over the years due to awareness, earlier detection and advancements in the diagnosis and treatment of the cancer. If you notice any lumps or changes to your breast, talk to your doctor.
Signs and Symptoms of Breast Cancer
If you notice any of these symptoms, talk with your doctor right away:
- A lump, hard knot or thickening in the breast
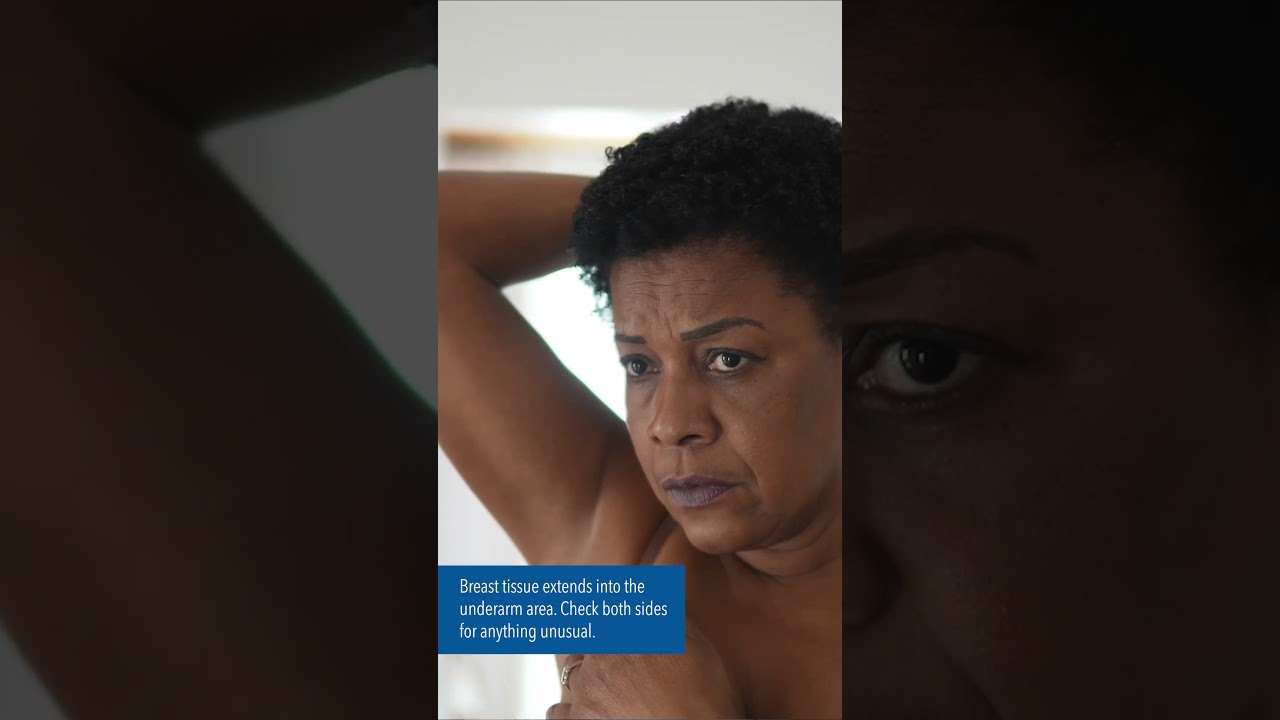
- A lump under your arm
- A change in the size or shape of your breast
- A breast that feels warm or swollen
- A change in skin color and texture such as dimpling, puckering or redness
- Nipple pain, tenderness or discharge, including bleeding
- A nipple turning inward or inverted
- Itchiness, scales, soreness or a rash on your nipple
People at Risk of Breast Cancer
- Assigned female at birth
- Began your menstrual periods before age 12 or entered menopause after age 55
- Over the age of 40
- Never had children or had your first child after age 30
- Have never breastfed
- Overweight or obese and not physically active
- Smoking or using tobacco in any way
- Drink alcohol in excess
- Are currently using or have recently used birth control pills
- Used hormone replacement therapy (HRT) with estrogen and progesterone for more than 10 years
- Have mutations of BRCA1, BRCA2, PALB2 or other genes
- Have a family history of breast, colorectal or ovarian cancer (if you have a family history of cancer, talk to your doctor about genetic testing)
- Had high-dose radiation therapy on your chest
- Have already had cancer in one breast or your chest
Breast Cancer Diagnosis
Different tests can be used to look for and diagnose breast cancer. If your doctor finds an area of concern on a screening mammogram, or if you have symptoms that could mean breast cancer, you’ll need more tests to confirm a diagnosis, such as:
- Diagnostic Mammogram
- Breast Ultrasound
- Breast MRI
- Breast Biopsy
Types of Breast Cancer
- Ductal Cancers
- Inflammatory Breast Cancer
- Lobular Cancers
- Metastatic Breast Cancer
- Triple Negative Breast Cancer
Ductal Carcinoma in Situ (DCIS) is a non-invasive breast cancer. Abnormal cells are found in the lining of the breast milk duct. These atypical cells haven’t spread outside of the ducts into the surrounding breast tissue. DCIS is an early cancer that’s highly treatable. If left untreated or undetected, it may spread into the surrounding breast tissue.
Invasive Ductal Carcinoma (IDC) is an invasive cancer where abnormal cancer cells that began forming in the milk ducts have spread beyond the ducts into other fatty parts of the breast tissue. Invasive cancer cells can also spread to other parts of the body. It’s sometimes called “infiltrative ductal carcinoma.” This is the most common form of breast cancer.
Inflammatory breast cancer (IBC) is a rare and aggressive type of breast cancer. IBC occurs when cancer cells infiltrate the skin and lymph vessels of the breast. IBC is harder to diagnose than other types of breast cancer and tends to occur in younger women. It also spreads more quickly than other types of breast cancer. Despite the name, inflammatory breast cancer is not caused by inflammation. Rather, the term refers to the inflamed appearance of the breasts.
Unlike many other types of breast cancer, inflammatory breast cancer doesn’t typically start with a distinct lump or tumor in the breast that can be felt or isolated. Instead, when the lymph vessels of the breast become blocked by breast cancer cells, symptoms begin to appear. These symptoms include areas of skin discoloration or rash on the breast, swelling, firmness, itching, nipple changes or discharge or swollen lymph nodes near the underarm or collarbone. There’s no clear cause of inflammatory breast cancer.
Lobular Carcinoma in Situ (LCIS) is not breast cancer. It’s a condition where abnormal cells are found in the lobules (milk glands) of the breast. The atypical cells haven’t spread outside of the lobules into the surrounding breast tissue. LCIS is highly treatable and rarely becomes invasive cancer. However, having LCIS in one breast increases the risk of developing breast cancer in either or both breasts.
Invasive Lobular breast cancer (ILC) is invasive breast cancer that begins in the lobules (milk glands) of the breast and spreads to surrounding normal tissue. It can also spread through the blood and lymph systems to other parts of the body. The stage of cancer impacts treatment and outcome.
Metastatic breast cancer (MBC) is Stage 4 breast cancer that’s spread from the original location in the breast to other areas of the body. When breast cancer recurs to another part of the body months or years after the initial breast cancer diagnosis and treatment, it’s called metastatic breast cancer.
There’s no cure for metastatic breast cancer, but more women live longer with the disease by managing it as a chronic illness with a focus on quality of life as a primary goal. The focus of treatment is to control the disease through continuous treatment and monitoring.
A diagnosis of triple negative breast cancer means the three most common types of receptors known to fuel most breast cancer growth — estrogen, progesterone and the HER2/neu gene — aren’t present in the cancer tumor. Since the tumor cells lack the necessary receptors, common treatments like hormone therapy and drugs that target estrogen, progesterone and HER2 are ineffective. Triple negative breast cancer is more aggressive and difficult to treat. Also, the cancer is more likely to spread and recur. The stage of breast cancer and grade of the tumor influence prognosis. Research is being done to create drug therapies that are specific for triple negative breast cancer.
Those most at risk for triple negative breast cancer include younger people, African Americans, Hispanics and those with a BRCA1 gene mutation.
Breast Cancer Treatment
Treatment depends on your type and stage of the breast cancer. In some cases, it’s necessary to remove the entire breast (mastectomy) or the abnormal portion of the breast (lumpectomy). Some treatments can work alone and some in combination with other treatments. Treatments include:
- Breast Cancer Surgery is performed by experienced breast surgeons and includes lumpectomies (removing a lump) and mastectomies (full or partial breast removal.)
- Chemotherapy drugs destroy cancer cells by stopping them from growing or reproducing.
- Hormone therapy alters hormone levels in the body to treat cancer cells.
- Immunotherapy enhances the body’s immune system to recognize and attach cancer cells.
- Radiation therapy uses high-energy radiation to damage the building blocks of cancer cells and stop them from growing or spreading. It can cause the tumor to shrink, and in some cases, die.
- Targeted therapy focuses on specific molecules or pathways involved in the growth and survival of caner cells, aiming to block their activity reducing growth and promoting cell death.
Who’s Who: Breast Cancer Care Team
- Primary care/OGBYN: Contact for initial suspicious breast lumps or concerns.
- Breast radiologist: Takes breast images for routine screenings or sudden concerns. May take biopsies.
- Care Coordinator/Nurse Navigator: Point of contact during your cancer journey.
- Surgeon: Takes biopsies and removes cancerous growths via surgical procedures.
- Oncologist: Oversees cancer treatment.
- Radiation oncologist: Develops and oversees personalized radiation treatment.
You may also work with the following team members during your cancer journey.
- Social worker: Provides emotional support and resources during a cancer diagnosis.
- Dietitian: Designs a personalized nutrition plan.
- Exercise specialist: Helps with lymphedema, strength, stability and overall physical wellness.
- Genetics professional: Conducts cancer risk assessment and genetic counseling, testing and education.
Breast Cancer Prevention
- Maintain a healthy weight by exercising and making healthy food choices
- Aim for at least 30 minutes of physical activity per day, 5 days a week
- Eat a variety of nutritious foods to keep your weight at a healthy level and avoid excess sugar, fat and processed foods
- Never smoke or use tobacco - if you do, quit
- Breastfeeding may lower a woman’s risk
- Limit alcohol intake. Alcohol is a known carcinogen, a substance capable of causing cancer. The more you drink, the greater your risk — even in small amounts.
- Aim for 7-9 hours of sleep each night and reduce stress
- Stay on top of cancer screenings - early detection saves lives
- Know your family history and talk to your doctor about genetic testing
Breast Cancer Videos


Breast Cancer Screening
- Most women of average risk will start mammogram screening in their 40s.
- Your primary care provider will talk with you about when to get started and how often is right for you. If you have a family history of breast cancer, please share this information with your doctor.
- In addition to mammograms, breast self-awareness is important. This means knowing how your breasts normally look and feel, which helps you notice any changes.
- If you’re a transgender individual, discuss specific breast cancer screening needs with your doctor.
Our Cancer Centers
Each cancer experience is unique, and that’s why our experienced cancer center teams are committed to using the latest treatments and clinical research to provide you with advanced care close to home.
