Younker Rehabilitation

The Leader in Physical Medicine and Rehabilitation
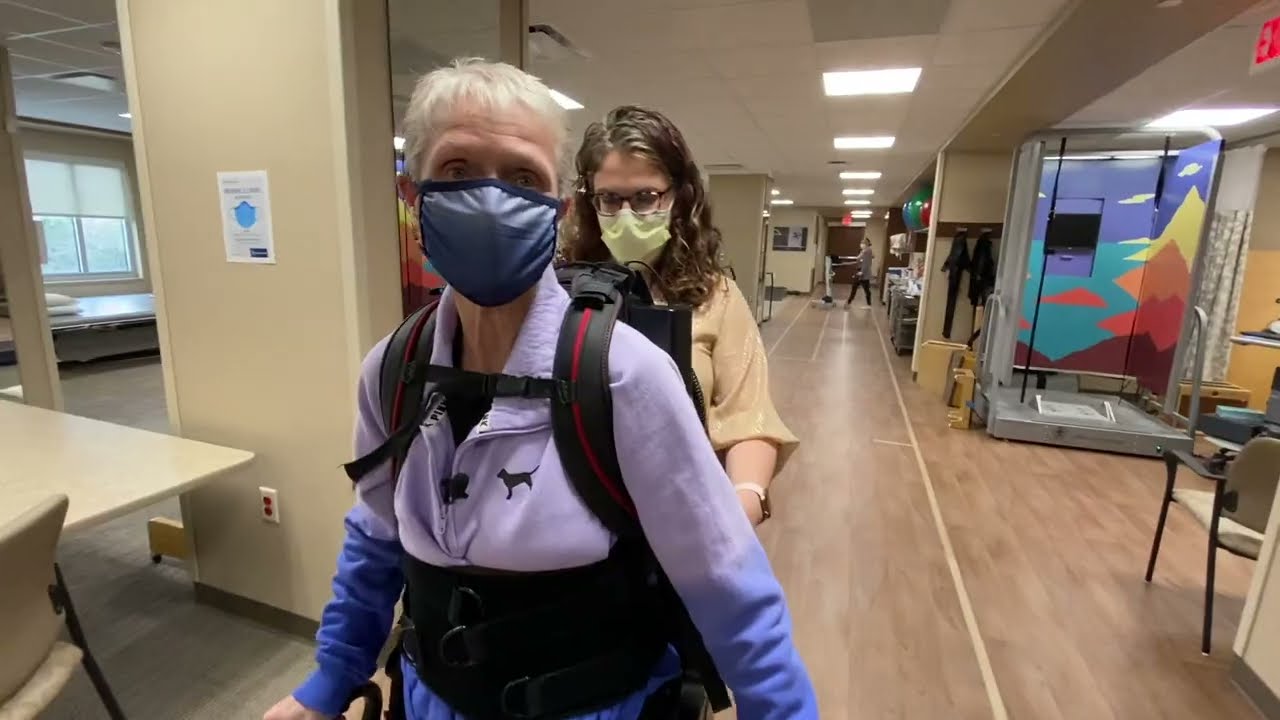
Younker Rehabilitation, a service of UnityPoint Health – Des Moines, is committed to helping you improve your ability to function and become as independent as possible. As a regional leader in the physical rehabilitation field, we offer an acute inpatient rehabilitation hospital that can manage complex patient needs as long as it does not impede on the patient's participation in their rehabilitation plan. We serve our patients throughout their physical rehabilitation journey, from an inpatient stay to outpatient rehabilitation at our Younker Rehabilitation Clinics, to therapy and physician care.
By providing highly specialized care, advanced treatment and cutting-edge technologies, we help individuals with spinal cord injury, brain injury, amputation, stroke, complex medical conditions, neurological diseases and musculoskeletal or orthopedic trauma to rebuild their lives.
Comprehensive Care
Our team works with you and your family to set goals for improved function and prepare you for a successful discharge. Our primary emphasis is on empowering you with the tools and education you will need to maximize the amount of function you can regain through rehab and work to address and overcome fear and anxiety that may interfere with daily living.
Physical Medicine and Rehabilitation Specialties
If you or a loved one has sustained a debilitating injury or illness, has complex medical conditions or experienced worsening of a chronic condition and is ready for an aggressive program of therapy and patient/family education to improve the quality of life, Younker Rehabilitation is here to help.
Choosing a Physical Medicine & Rehabilitation Facility
Younker Rehabilitation is an acute rehabilitation unit specializing in complex medical and therapeutic needs. As part of UnityPoint Health - Des Moines and an extensive healthcare system, Younker Rehabilitation offers services to meet a variety of rehab or medical needs both while you are an inpatient rehabilitation patient and following your discharge. Your rehab may continue in one of our many outpatient therapy clinics or a network of physician offices. We also offer assistance with medical equipment, home care and numerous other options. As part of UnityPoint Health, we provide a network of healthcare services throughout Iowa and parts of Illinois and Wisconsin.
For a referral to Younker Rehabilitation, contact us at DM_RReferrals@unitypoint.org or call (515) 241-4499.
Award Winning Facility
Younker Rehabilitation has been a recognized leader in providing a patient-centered rehabilitation experience since opening in 1959, successfully assisting patients and families to reach their optimal level of function following illness or injury. Younker Rehabilitation has been accredited by the Commission on Accreditation of Rehabilitation Facilities (CARF) since 1985. This means we demonstrated to a team of surveyors during an on-site visit our commitment to offering programs and services that are accountable, measurable and of the highest quality.
- Our facility is designed with healing colors and themes of nature, including our own oak tree, a symbol of strength and endurance to support Younker Rehabilitation's holistic person-centered approach to better serve our patients and families.
- We have brought natural elements into a neighborhood setting. Our therapy gym, Younkerville, is a park-like area with a walking track, benches, studios for treatment sessions and a mock apartment that simulates real-life situations, in addition to state-of-the-art equipment.
- We have 23 private in-patient rehabilitation rooms with accommodations for family and a large accessible bathroom, as well as a transitional room for families to use as they prepare for discharge to home.
- The community center offers areas for dining, a full kitchen, a pool table and games for recreation therapy and socialization.
Knowledgeable Rehabilitation Team
Our team of more than 60 clinicians and support staff have a combined 500+ years of rehabilitation experience. Our interdisciplinary team works together to maximize our patients' independence and safety through individualized treatment and education. Every member of our team works collaboratively and communicates openly with you to meet your needs and achieve your goals. Many of our clinicians hold specialty certifications and advanced degrees. We have nine Certified Brain Injury Specialists (CBIS) on staff, and several of our nurses are Certified Rehabilitation Registered Nurses.
Full Kitchen
Our kitchen was designed to include all of the things found in a typical kitchen to allow our patients to practice homemaking in a real-world environment. The full kitchen has an oven, refrigerator, microwave, toaster, coffee pot and dishwasher.
- Occupational therapists will work with patients in the kitchen, practicing reaching into cupboards, maneuvering a walking device while transporting food, learning the use of one-handed techniques and working on safety while using a stove, oven or while cutting.
- A patient may practice heating up a microwave meal to improve their ability to read and follow instructions. A patient may also plan a meal, make a shopping list, and prepare this meal to work on sequencing, problem-solving and other higher level thinking skills.
- Speech therapy may use the kitchen to identify common items and how they are used.
- Physical therapy may lay out an outline of the barriers that may exist in a patient's own kitchen at home so that the patient can practice maneuvering around them during a functional task. They may also work with a patient to retrieve items from various heights to work on balance.
Laundry Room
There is a laundry room set up in the unit to work on the physical and cognitive skills required for this daily living task. The therapists may work together on the goals of:
- Balance and strength to stand while using the washer or transferring clothing to the dryer.
- Problem-solving skills to decide what needs to be washed and what settings to use.
- Memory and recall to remember to return to move laundry to the dryer or to retrieve laundry after finished.
- Use of adaptive equipment to assist if a patient is unable to stand or reach to access all items needed in the laundry room.
This apartment-like room allows patients and caregivers to practice the skills learned in therapies and with nursing in an environment similar to at home. While the patient and caregiver are encouraged to manage bathroom tasks, take him/herself to therapies, and practice medication management by calling staff when it is time for medications, the staff is always available to assist, if needed. This allows for a safe trial before going home to determine any possible situations which may occur when a patient is trying things on their own and/or allowing family members to practice being the caregiver before leaving the hospital.
Discharge can be a stressful time for patients and families, and the use of either the transition room or modified transition in the patient's hospital room can help to alleviate many of the worries that can occur.
The transition room features:
- Queen size bed
- Fridge for simple meal prep
- Table and chairs for family style meals
- Pull-out futon couch for family members or caregivers
In the therapy gym, we have a dedicated room set up like an apartment. It has a full size 'normal' bed, dresser, closet, functioning storm door, front door, window, couch, recliner chair and vacuum. These items allow therapy to practice in more standard environments tasks such as:
- Getting up from a fall
- Getting on and off a regular bed
- Making a regular bed
- Putting clothes away in a dresser or closet
- Vacuuming the floor
- Opening the front door
- Practicing entering over doorways
- Getting on and off a couch
After an injury or illness, families and patients may need to look at their home to determine if changes are required to make the space more accessible or safe. At Younker Rehabilitation, we know this can be a daunting task for a family who may not know where to start.
Our therapists work with patients and families to determine discharge plans, including adaptations required to allow the patient to return home. The therapist will ask families for pictures or descriptions of their home (number of floors, how many steps, etc.). A questionnaire has been put together by our therapists that helps families know what areas should be measured in the home. The family member then returns the questionnaire to therapy so that this information can be incorporated into the treatment plan. For example, therapists can set up a simulation of the patient's bathroom at home using the measurements provided in the questionnaire, allowing a patient to practice transfers as they would be done at home.
Additionally, this allows therapists and families to identify any changes or equipment that may make the patient's return to home more successful. Some modifications may include: grab bars, ramped entry, and shower chair/bench.
Interdisciplinary Team Approach
As an interdisciplinary team, each caregiver reinforces the teaching done by other health care disciplines. Our dedicated team works together to improve the functional independence and quality of life for our patients. We partner with you and your family to set goals for improved function and prepare you for a successful discharge. The rehabilitation team meets formally each week to share progress toward goals, discuss any barriers and make new goals for the coming week. Discharge planning occurs both at this meeting, after initial evaluation by team members and throughout a patient's stay.
Meet the Medical Director of Younker Rehabilitation
Physical Medicine and Rehabilitation Team
A physiatrist is a physician who specializes in physical medicine and rehabilitation. Our physiatrists meet with their patients regularly and direct the rehabilitation plan. Each patient at Younker Rehabilitation has a physiatrist who leads the patient and family conference, a weekly team conference and regular visits with the patient.
Our team of physical therapists has over 60 years of combined experience. Physical therapists and physical therapist assistants provide physical therapy rehabilitation services to improve function, focusing on gait training (walking), mobility, pain control, strengthening, motor planning, balance and coordination activities.
With more than 90 combined years of certified rehabilitation nursing experience, our nurses have the skills and knowledge to assist patients with new or worsening disability and/or chronic illness to attain and maintain maximum function. The nurses assist patients in adapting to an altered lifestyle, while providing a therapeutic environment for patients and their family's to develop skills to assist the patient in achieving a safe transition to the community.
Our nurses collaborate with the interdisciplinary team to design and implement the rehabilitation plan. Nursing interventions and care are holistic and evidence-based and include self-care and promotion of physical, psychosocial, and spiritual health. Some areas of rehabilitation nursing expertise include: skin care and wound prevention, medication management, disease process education, diabetes management, bowel and bladder management, care coordination and discharge planning.
Rehabilitation Therapies & Services
We specialize in rehabilitation services for individuals aged 14 and older who require:
- An inpatient hospital setting with 24-hour rehabilitation registered nurse care.
- At least two therapy disciplines (physical therapy, occupational therapy and/or speech therapy) for three hours per day, five days per week.
- A rehabilitation physician (physiatrist) to lead the interdisciplinary team and assess progress and goals via face-to-face visits with the patient three times per week.
- Our facility also offers a full recreation therapy program for its residents.
If the patient is cognitively unable to make decisions, a family member or legal representative must be identified to speak on their behalf prior to the decision for admission. Patients and families are the focus of our physical rehabilitation team. We know you have experienced a life-changing event and your family is important in your recovery.
Therapies
Physical therapists work with patients so they can maneuver within their environment more independently. This may include:
- Getting in and out of bed
- Accessing the shower/tub and toilet
- Going up and down stairs
- Getting in and out of chairs and other furniture
- Getting in and out of the car
A physical therapist who is a wheelchair specialist will evaluate patients to determine the best wheelchair or other assistive mobility device. Our therapists are skilled in fitting the best solution to each patient, whether it is a manual wheelchair or customized power wheelchair. Pressure mapping may be performed to determine what cushion is best for each patient to reduce potential sources for pressure ulcers or wounds.
Our therapists have many tools they can use in your physical rehabilitation. When working with patients who have had a stroke, we work to improve strength and control of parts of the body that need physical therapy.
- Electrical stimulation is sometimes used to "facilitate" or excite the muscle, so it contracts more fully during muscle training.
- We have the Bioness L300, which is a device that delivers electrical stimulation in a way that assists with gait training, or walking.
- An electrical stimulation bike (RT300 Arm and Leg FES) may be used to strengthen and retrain muscles after a stroke, or spinal cord injury.
- Patients who are beginning to walk and need support may work with the Lite Gait, which is an overhead harness system to reduce the weight bearing through the legs during walking.
Our occupational therapy programs focus on techniques to become more independent with daily living tasks. This includes commercially available adaptive equipment or equipment fabricated for a specific person's needs.
Occupation therapists specialize in helping patients regain use of their arms and hands.
- Using equipment like the Deltoid Aide or the SaeboMAS allows the patient to work on strengthening and control of the arm even if they are not yet able to lift against gravity.
- Electrical stimulation may be used to strengthen a muscle contraction during neuromuscular training.
- We may fit patients with a lightly compressive glove, position the arm on an elevating arm rest or perform massage to reduce swelling in the hand.
After an injury to the brain or a stroke, an occupational therapist may screen the patient for visual and perceptual changes.
- We involve both the patient and their family in our visual assessments to help educate everyone about how to make the home environment easiest to navigate for the patient.
- We'll help to maximize vision, train the patient in methods to reduce the effect of a visual field cut or neglect or inattention to one side, and work toward restoration or compensation for visual/perceptual changes.
- We use a variety of assessments to look at your visual skills, like the Dynavision D2™. The Dynavision helps with visual skills, weight shifting, use of one or both arms and improving attention and concentration.
Sometimes simple changes to the home environment can improve a patient's vision. We make suggestions to improve lighting so our patients can avoid harsh glares, see books and magazines more clearly and walk feeling safe and independent when they return home. Our occupational therapists work with patients, families and staff to see what types of aides they might need. We call these, "environmental controls and assistive technology." Sometimes these aides are high-tech, like a voice-activated controller for lights, TVs and phones. Other devices are very simple, such as a pointer for people who have trouble bending or using their hands and arms.
Speech therapists, speech-language pathologists, evaluate and treat communication and swallowing disorders.
- The speech therapist will sometimes do a test called a videofluoroscopy with a radiologist present. This records a person swallowing, which allows the speech therapist and radiologist to see if the patient is swallowing safely. Based on the test's findings, speech therapists recommend food and liquid with the safest consistency for the patient's differing needs. Mealtime observations give us the chance to monitor patients and teach or help them work toward feeding themselves.
Much of a speech therapist's time is spent assessing cognition.
- Cognition, or thinking skills, can be affected by an injury to the brain such as anoxia, seizures or stroke. Cognition can also be affected by dementia, alcohol or drug use/abuse, medications and metabolic imbalances.
- Speech therapists plan an individualized program to focus on improving thinking skills so patients can quickly return to caring for necessary things like managing medication or paying bills.
A stroke or brain injury sometimes changes how people talk, sound or receive information from others. It may be hard to understand them when they speak or read aloud.
- Speech therapists train and educate patients in the use of techniques and exercises that help them maximize or regain their ability to communicate. iPad programs may be used to work on certain cognitive skills or to compensate for cognitive losses.
Understanding Our Levels of Patient Care
Level of care is used to describe the type and intensity of medical care you will receive. The determination of your level of care is made by you and your family, the admitting facility and/or physician and insurance provider. You are the center of our team. It's important to understand the different levels of care and the specialized treatment, care, services and equipment provided at each level. During your time with us, you may receive one level of care, or transition to a different level depending on your condition. We strive to bring the best outcome for every patient, every time, with our patient-centered and physician-driven system of care.
Levels of Care
Amount of Rehabilitation Therapy Provided
- Customized care to fit patients needs depending on diagnosis, severity of injury, medical complications and rehabilitation goals.
- Patients are admitted into this program after a consultation with the rehabilitation referral team.
- Patients must be able to tolerate three to five hours of therapy a day, five days per week, and be in need of at least two therapy services and rehabilitation nursing.
- Younker Rehabilitation has recognized the importance of feeling at home when receiving your therapies, and helping achieve realistic results to help you regain independence.
Nursing Care
- Requires 24 hours per day of specialized Rehabilitation Nursing.
- Examples include: Patient/family education for managing life with new physical impairments, education for managing altered bowel and bladder function, urinary self-catheterization, medication management and skin care.
- Reinforcing newly learned skills in safety, mobility and self-care.
- Our team meets weekly to address the patient's plan of care, barriers and process to achieve the highest level of a recovery.
Physician Care
- Physical Medicine & Rehabilitation physician actively involved in planning treatment and monitoring patient progress. Physician completes a face-to-face visit three times per week.
- Communication with patient, family and caregivers is an important part of the process.
Likely Candidates
- Individuals 14 years of age and older.
- Individuals who have recently been affected by stroke, brain injury, spinal cord injury, traumatic injury, neurological condition or other disabling condition or disease process.
- Individuals living with a disability who have had a recent change in condition, injury or illness that has impacted their ability to manage day-to-day activities.
- Successful rehabilitation includes the active involvement of supportive family and friends. Patients who may be unable to vocalize personal needs will require a family member or legal representative to speak on their behalf.
The Younker Rehabilitation inpatient unit is located at UnityPoint Health - Iowa Methodist Medical Center. There is also a satellite unit at Iowa Lutheran Hospital.
Amount of Rehabilitation Therapy Provided
- Customized therapy for patients based on need.
- Care delivered in the patient's home and is focused on creating safety and independence.
- Therapy visits vary in length and each discipline visits 1-3 times per week based on patient need.
- Therapy often focuses on fall reduction and home safety measures.
- Services are provided in the patient's home.
Nursing Care
- Nursing visits 1-7 times per week based on patient need.
- Skilled nursing services including IV therapy, wound care, catheter care and ostomy care.
- Teaching patients with new diagnoses or other changes in health status.
- Observation and assessment of chronic conditions.
Physician Care
- Home health Plan of Care is developed in partnership with the patient's primary care provider.
Likely Candidates
- Patient's basic needs are met at home through self or other caregiver.
- Patient requires nursing or therapy to recover to prior level of function or to help manage a chronic condition.
- Patient is unable to travel to outpatient therapy.
Amount of Rehabilitation Therapy Provided
- One to three hours per day, therapies dependent upon patient need.
- Two to three days per week.
Nursing Care
- None
Physician Care
- Routine office visits with primary care provider, and specialists such as orthopaedic surgeon, physical medicine and rehabilitation, neurologist and other providers that direct your care.
Likely Candidates
- Patients whose physical disabilities and medical problems are stable enough to live in their own homes and can travel to get their treatment.
- Many patients who have been treated in their provider's office, the hospital, inpatient rehabilitation or skilled nursing may transition their recovery plan to this level of care setting.
Patient Recovery Stories



Outpatient Clinics
